What Is the Microbiome?
The human gut microbiome represents one of the most fascinating and complex ecosystems on our planet. This invisible community of microorganisms inhabiting our digestive tract has emerged as a critical factor in human health research in recent years. The gut microbiome refers to the collective genomes of the trillions of microorganisms residing within our intestinal tract, including bacteria, archaea, fungi, and viruses, with bacteria making up the largest portion.
The human gastrointestinal tract houses an estimated 100 trillion microorganisms, containing over 1,000 different species. Remarkably, the genetic contribution of these microbes far exceeds our own human genome – while humans have approximately 23,000 genes, the microbiome contributes an estimated 3 million genes, making it 150 times larger than the human genome.
Composition of the Gut Microbiome
The healthy human gut microbiome is dominated by four main bacterial phyla:
- Bacteroidetes – typically the most abundant phylum in healthy adults, making up approximately 70% of the gut microbiota
- Firmicutes (also called Bacillota) – the second most abundant phylum, comprising about 20% of gut bacteria
- Actinobacteria – constituting around 2% of the gut microbiota
- Proteobacteria – making up approximately 2% of gut bacteria
While these phyla represent the majority of gut bacteria, other phyla including Fusobacteria and Verrucomicrobia are also present in smaller amounts. Within these phyla, the genus Bacteroides is typically the most abundant, followed by various genera from the Firmicutes phylum such as those in the families Lachnospiraceae and Ruminococcaceae.
It's important to note that every individual's microbiome is unique – like a fingerprint – and is influenced by numerous factors including genetics, diet, environment, lifestyle, medication use, and age. This diversity means there is no single "ideal" microbiome composition, but rather a spectrum of healthy configurations.
Development of the Microbiome
The development of our gut microbiome begins at birth. During vaginal delivery, infants are exposed to the mother's vaginal and intestinal microbiota, providing the first microbial colonizers of the infant gut. Babies born via C-section initially acquire different microbes, primarily from the skin and hospital environment.
Breastfeeding further shapes the infant microbiome, as breast milk contains prebiotics (oligosaccharides) that specifically nourish beneficial bacteria like Bifidobacteria. The introduction of solid foods represents another significant shift in microbial composition, with greater diversity developing as the diet expands.
By around age three, the gut microbiome begins to resemble an adult configuration, though it continues to evolve throughout life. During adulthood, the microbiome remains relatively stable in healthy individuals, with certain shifts occurring as we age.
Functions of the Gut Microbiome
The gut microbiome performs several vital functions that benefit human health:
Nutrient Metabolism and Energy Harvest
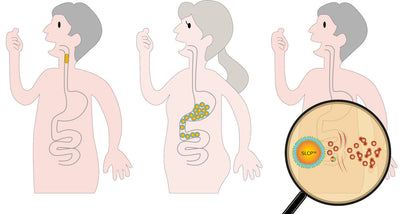
A key function of gut microbiota is the fermentation of dietary fibers and resistant starches. Through this process, bacteria produce short-chain fatty acids (SCFAs) – primarily acetate, propionate, and butyrate – which provide energy for intestinal cells and help regulate metabolism.
Additionally, gut bacteria synthesize essential vitamins, including vitamin K and several B vitamins, and enhance the absorption of minerals like calcium, magnesium, and iron.
Protection and Barrier Function
The gut microbiome creates a natural barrier against potentially harmful microorganisms by occupying ecological niches and producing compounds that maintain a balanced intestinal environment. This "colonization resistance" helps maintain gut homeostasis.
Immune System Support
The gut microbiome plays an important role in supporting immune function, helping to educate the immune system from early life through adulthood. This ongoing communication helps maintain appropriate immune responses.
Gut-Brain Connection
Research has identified bidirectional communication between the gut microbiome and the brain, often called the "gut-brain axis." Through various pathways, including neural connections and metabolites, the gut microbiome may influence various aspects of brain function.
Factors Affecting the Gut Microbiome
Multiple factors influence the composition and function of the gut microbiome:
1. Diet
Diet is perhaps the most significant modifiable factor affecting gut microbial composition. Different dietary patterns promote distinct microbial communities:
- Fiber-rich diets (high in fruits, vegetables, whole grains, legumes) support diverse microbiota and increased SCFA production
- Western diets (high in animal protein, fat, and simple carbohydrates) are associated with reduced microbial diversity and altered metabolic outputs
- Specific dietary components like polyphenols (found in berries, tea, and red wine) and fermented foods can selectively enrich beneficial bacteria
Dietary changes can induce rapid shifts in the microbiome, with alterations detectable within 24-48 hours of major dietary changes.
2. Antibiotics and Medications
Antibiotic use profoundly affects the gut microbiome:
- Broad-spectrum antibiotics can reduce microbial diversity and abundance
- Effects can persist for months after treatment ends
- Repeated antibiotic exposure may lead to permanent alterations in microbial communities
Other medications, including proton pump inhibitors, metformin, and non-steroidal anti-inflammatory drugs, can also influence microbiome composition.
3. Age
The microbiome naturally changes across the lifespan:
- Infant microbiomes are less diverse and more variable than adult microbiomes
- Adult microbiomes remain relatively stable during middle age
- Older adults often experience reduced diversity and shifts in dominant bacterial groups
4. Exercise
Physical activity positively influences the gut microbiome:
- Regular exercise is associated with increased microbial diversity
- Exercise promotes beneficial bacteria that produce SCFAs
- The magnitude of exercise effects may depend on intensity, duration, and type of activity
5. Stress and Sleep
Psychological stress and sleep disturbances can alter the gut microbiome:
- Chronic stress may reduce beneficial bacteria and increase potentially harmful species
- Poor sleep quality correlates with less favorable microbial profiles
- Stress management and good sleep hygiene may support microbiome health
Supporting Gut Microbiome Health
Several evidence-based approaches can promote a healthy gut microbiome:
1. Dietary Strategies
- Increase dietary fiber intake: Aim for diverse plant foods (fruits, vegetables, whole grains, legumes, nuts, and seeds) to provide various types of fiber that feed different beneficial bacteria
- Include fermented foods: Yogurt, kefir, sauerkraut, kimchi, and other fermented foods may introduce beneficial microbes
- Limit ultra-processed foods: Highly processed foods often contain ingredients that may adversely affect beneficial gut bacteria
2. Prebiotics
Prebiotics are non-digestible food components that selectively stimulate the growth and/or activity of beneficial gut bacteria. Rich sources include:
- Chicory root
- Jerusalem artichokes
- Garlic
- Onions
- Leeks
- Asparagus
- Bananas
- Oats
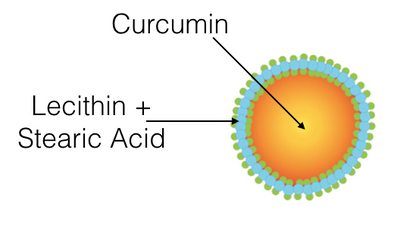
3. Lactic Ferments and Beneficial Microorganisms
Live beneficial microorganisms, when consumed in adequate amounts, can enhance microbiome diversity and balance. Well-researched beneficial microbial strains include:
- Lactobacillus species
- Bifidobacterium species
- Propionibacterium
- Saccharomyces boulardii (a beneficial yeast)
4. Lifestyle Factors
- Regular physical activity: Aim for at least 150 minutes of moderate-intensity exercise per week
- Stress management: Practices like meditation, yoga, and deep breathing can help reduce stress
- Adequate sleep: Prioritize 7-9 hours of quality sleep per night
- Judicious antibiotic use: Use antibiotics only when necessary and as prescribed
Conclusion
The gut microbiome represents a fascinating frontier in health research. As our understanding deepens, it becomes increasingly clear that these microbial communities play pivotal roles in human health. While there is no single "perfect" microbiome, diversity and functional capacity appear to be hallmarks of a healthy gut ecosystem.
Supporting gut microbiome health through diet, lifestyle, and targeted interventions offers promising avenues for promoting overall wellness. As research continues to evolve, our appreciation of these microbial partners and their contributions to human health will undoubtedly expand, opening new possibilities for microbiome-based approaches to health.
References
- Mohajeri MH, Brummer RJM, Rastall RA, et al. The role of the microbiome for human health: from basic science to clinical applications. European Journal of Nutrition. 2018;57(1):1-14.
- Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486(7402):207-214.
- Rinninella E, Raoul P, Cintoni M, et al. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms. 2019;7(1):14.
- Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. BMJ. 2018;361:k2179.
- Donohoe DR, Garge N, Zhang X, et al. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell Metabolism. 2011;13(5):517-526.
- Fusco W, Lorenzo MB, Cintoni M, Porcari S, Rinninella E, Kaitsas F, Lener E, Mele MC, Gasbarrini A, Collado MC, Cammarota G, Ianiro G. Short-Chain Fatty-Acid-Producing Bacteria: Key Components of the Human Gut Microbiota. Nutrients. 2023 May 6;15(9):2211.